In recent years, numerous headlines have drawn attention to rising rates of throat cancer—specifically oropharyngeal cancer—in various parts of the world, including the United Kingdom and the United States. Much of this discussion focuses on human papillomavirus (HPV), a common infection transmitted through intimate contact, including oral sex. When certain strains of HPV persist in the body, they have the potential to contribute to the development of certain cancers. Researchers, including Dr. Hisham Mehanna from the University of Birmingham, have studied these trends and highlighted the link between HPV and oropharyngeal cancer. However, the topic has occasionally been presented in sensational ways, causing confusion or fear. This article aims to delve into the existing research, clarify what is currently known, and provide context around HPV, oropharyngeal cancer, and the potential influence of oral sex on these findings—while avoiding exaggeration or misinformation.
Defining Oropharyngeal Cancer
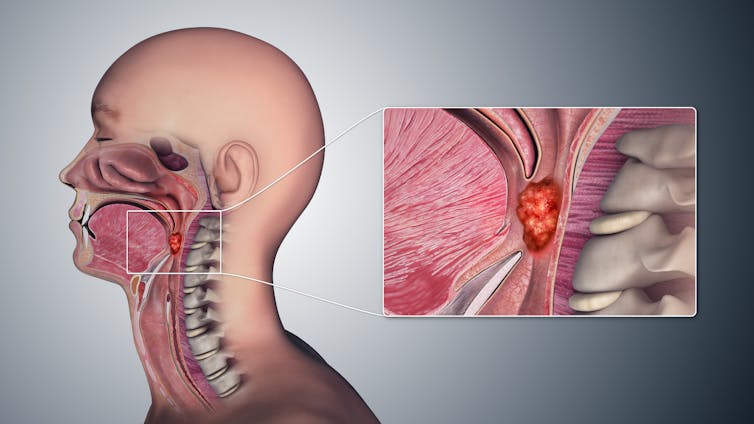
Oropharyngeal cancer refers to malignancies that occur in the oropharynx, the area of the throat directly behind the mouth. This region includes the tonsils, the soft palate, and the base of the tongue. Individuals with oropharyngeal cancer may experience a variety of symptoms such as persistent sore throat, difficulty swallowing, unexplained weight loss, or lumps in the neck. Historically, the leading risk factors for oropharyngeal cancer were primarily heavy tobacco use and excessive alcohol consumption. Yet in the past few decades, a noticeable shift has occurred in many countries, with HPV now implicated in a growing proportion of these cancer cases.
The Role of HPV
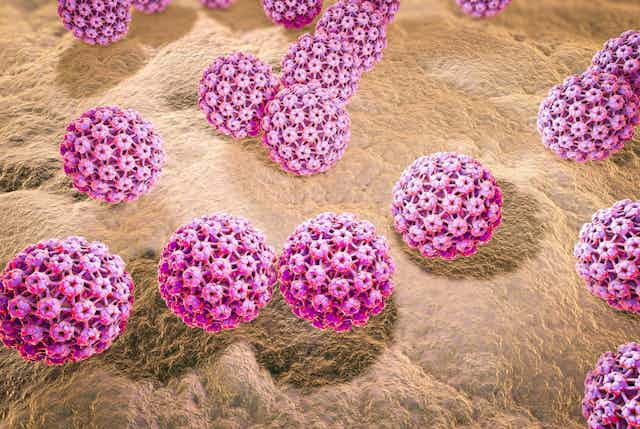
Human papillomavirus (HPV) is actually a family of more than 100 related viruses. While the majority of HPV types cause no serious harm and often clear from the body without intervention, certain high-risk strains can lead to the development of cancers, including cervical, anal, and oropharyngeal cancers. The virus is transmitted through skin-to-skin contact, typically during sexual or intimate encounters. Oral sex can be a route for transmitting HPV to the oropharynx, where it may potentially contribute to cancer formation if the infection fails to clear.
When discussing HPV-related throat cancer, it is common for scientists to focus on “HPV type 16,” one of the high-risk variants frequently connected to malignancies. If an individual acquires this high-risk HPV strain in the oral or throat region, the body often clears the infection naturally within one to two years. For a small percentage of people, however, the virus persists, potentially leading to cellular changes that, over many years, develop into cancer. This progression is neither immediate nor universal; it is dependent on a variety of factors, including genetic predispositions, lifestyle, immune system effectiveness, and overall health status.

Dr. Mehanna’s Observations
Dr. Hisham Mehanna, noted for his work on HPV-related cancers, has commented on the substantial increase in oropharyngeal cancer in Western countries. He identifies HPV as a primary driver behind this trend in many cases. Some articles summarize his remarks by suggesting that oral sex is “fueling” an epidemic of throat cancer. It is accurate that Dr. Mehanna and other researchers point to HPV transmission through oral contact as a significant factor in some oropharyngeal cancers. However, it is important to emphasize that saying “oral sex is now the main cause of throat cancer” can oversimplify a multifaceted issue. Yes, the prevalence of HPV-positive oropharyngeal cancers has risen considerably, and oral sexual contact is one way HPV can be transmitted. But other lifestyle factors and risk enhancers—such as smoking, heavy alcohol use, and overall immune health—remain relevant.
Moreover, while some experts have noted that rates of HPV-related oropharyngeal cancer have, in certain regions, outpaced the frequency of cervical cancer cases, each of these malignancies has its own epidemiological trends, screening options, and distinct risk factors. A direct comparison of these numbers does not automatically denote cause and effect; rather, it underscores that HPV can cause significant health issues affecting people of all genders, beyond the commonly known link with cervical cancer.
Risk Factors and Oral Sex Partners
One frequently cited statistic suggests that individuals with a higher number of lifetime oral sex partners face an increased risk of developing HPV-related oropharyngeal cancer. For instance, some studies have found that having six or more oral sex partners may raise the likelihood of oropharyngeal cancer by more than eightfold compared to those with fewer or no such partners. These findings serve as a reminder that sexual activity—particularly unprotected and with multiple partners—can elevate the chance of acquiring a persistent high-risk HPV infection in the throat region.
However, risk is not destiny. Many individuals who have had multiple partners do not develop cancer, just as some who have had fewer partners might. The immune system successfully clears the majority of HPV infections, and other factors—such as genetics, tobacco use, and overall health—also influence cancer risk. The data underscores the value of awareness, prevention efforts, and open conversations about sexual health.
Understanding the Body’s Response
In most cases, the human body’s immune system eliminates HPV infections over time. Whether the virus is located in the cervix, throat, or another anatomical site, immune cells often identify infected cells and eradicate them, preventing the virus from causing lasting harm. It is only when certain strains linger that abnormal tissue growth can progress into precancerous lesions and eventually malignancies. Researchers are actively investigating why persistent infections occur in some individuals but not in others. Hypotheses involve genetic differences, immune system deficiencies, lifestyle factors like smoking, and overall health.

Prevention and Vaccination
When considering HPV-related cancer prevention, one of the most impactful measures is vaccination. The HPV vaccine, recommended in many countries for adolescents and sometimes for adults up to a certain age, protects against the most dangerous strains of HPV, including type 16. Many health organizations have observed a significant decline in HPV-related cervical precancers among vaccinated populations, suggesting the vaccine also holds promise for reducing rates of HPV-associated oropharyngeal cancers in the future.
Safe sexual practices, including consistent condom or dental dam use, may also lower the risk of HPV transmission during oral sex. While these methods are not 100% effective against all forms of HPV (since the virus can infect areas not covered by barriers), they can still offer a degree of protection and overall risk reduction. Furthermore, limiting one’s number of sexual partners and maintaining open communication about sexual health are sensible approaches to reducing transmission risks.
Screening and Early Detection
Unlike cervical cancer, for which pap tests and HPV co-testing are standard methods of early detection, there is no widely adopted screening protocol for HPV-related oropharyngeal cancers. Currently, most oropharyngeal tumors are diagnosed when individuals develop symptoms or when irregularities are discovered during dental or medical examinations. Some signs that warrant further investigation include a persistent sore throat, difficulty swallowing, earaches, enlarged lymph nodes, or lumps in the neck. Since early detection improves treatment outcomes, prompt medical evaluation for these symptoms is advisable.
Healthcare providers, including dentists and dental hygienists, can play an essential role in early detection by examining the mouth and throat for suspicious lesions. This underscores the value of regular checkups not only for dental hygiene but also for broader oral and oropharyngeal health monitoring.

Challenging Myths and Misinformation
Given the complexity of HPV transmission and oropharyngeal cancer, it is crucial to approach the subject with both nuance and caution. Headlines that proclaim “Oral sex is now the main cause of throat cancer” may oversimplify a multi-factorial issue. While scientists like Dr. Mehanna do point to HPV acquired through oral sex as a significant contributor to the rise in certain throat cancers, this phrase alone can obscure the role of other risk factors and overshadow the broader context of prevention and healthcare strategies.
Additionally, stating that HPV is the “main cause” of all throat cancers neglects the fact that tobacco, alcohol, and other factors remain relevant contributors to oral and throat malignancies. A person who smokes heavily or consumes large amounts of alcohol is at an increased risk of developing oropharyngeal cancer, whether HPV is present or not. Likewise, a person with zero history of tobacco or alcohol use can still develop HPV-related oropharyngeal cancer if they carry a persistent high-risk strain. Thus, it is best to see this issue as multi-layered and to encourage informed, balanced discussions.
The rise in HPV-related oropharyngeal cancer underscores the evolving nature of cancer epidemiology and the importance of ongoing research. Vaccination efforts, public health education, and transparent discussions about safe sexual practices can all serve to reduce the incidence of these cancers over time. Being proactive—whether by scheduling routine medical evaluations, engaging in protective behaviors, or seeking timely advice for persistent symptoms—remains vital.
Ultimately, the link between HPV, oral sex, and throat cancer exists, but it is just one part of a broader, nuanced picture. By replacing sensational headlines with informed dialogue, individuals gain the tools to protect themselves and their loved ones, ensuring that valid scientific findings spur thoughtful awareness rather than unwarranted panic.
